

You’re not going to believe the truth behind online doctor consultations! This digital shift in healthcare isn't just a pandemic fad—it’s the future. What's more, the realities of telemedicine are much more compelling than you might think.
As we move further into the digital age, telemedicine solves longstanding healthcare issues like access and affordability. So, why is this transformation more crucial now than ever before? The answer might surprise you! And just wait until you learn what the experts are predicting next!

Did you know that telemedicine services have surged by over 600% in the last year alone? This unprecedented leap is changing how we perceive healthcare, but that’s not even the wildest part. Many patients have transitioned to digital health tools, reporting saved time, money, and quicker access to care. The surprising bit? Even healthcare professionals themselves are amazed at the benefits.
However, the appeal of online doctor consultations isn't just about convenience. It’s also fostering a new kind of relationship between doctors and patients. With real-time data and digital tools at their fingertips, patients are more engaged than ever before. You might expect this to be the tipping point, but there’s even more to this evolving narrative…
Ever wondered about how much deeper this transformation goes? What happens next shocked even the experts and rewires our preconceptions. Are you ready to uncover the layers beneath telemedicine’s flashy surface?
At first glance, telemedicine seems to offer just a convenient alternative to in-person visits. But dive a little deeper, and you'll see much more at play. Patients benefit from enhanced privacy and reduced stigma, especially those requiring mental health support. Virtual environments offer a sense of security that traditional settings often lack. What most don’t realize is how extensive the benefits can be when privacy is a top priority.
Additionally, telemedicine is bridging geographic gaps like never before. Patients from rural areas, who previously struggled to find specialists, now have access to top-tier medical advice with a few clicks. This geographical democratization is a game-changer; however, what’s more surprising is the domino effect this accessibility is triggering.
Remote consults are also shining a spotlight on secondary costs that frequently go unnoticed. Without travel expenses, time off work, or childcare needs for appointments, the cumulative savings are substantial. Yet, there’s more—some hidden costs are cleverly disguised as practical gains that might astonish even the most skeptical of healthcare critics.
What comes as a revelation to many is the change in patient engagement. Data-driven approaches have led to smarter healthcare choices, with patients actively participating in their own wellness plans. But there's one more twist to this unfolding story that’s changing the dynamics of healthcare forever…
The promise of a secure and private digital space enhances the telemedicine appeal. With end-to-end encrypted platforms, patients can discuss sensitive concerns without fear of eavesdropping or data breaches. Yet, what you might not expect is the role this privacy plays in patient honesty, leading to better diagnoses and outcomes.

Interestingly, studies indicate that patients are more likely to be forthcoming in telemedicine settings. The virtual barrier seems to translate into an openness not present in face-to-face encounters. This counterintuitive finding leads experts to wonder about the future of in-person consultations. Could it become standard practice to introduce online options for difficult conversations?
The tech advancements behind telemedicine go hand in hand with top-notch security protocols. But these aren't just ordinary measures; some platforms employ tactics straight out of a spy movie to ensure data protection. This high-stakes approach raises an essential question—how far is too far in safeguarding patient information?
The implications of this secure environment motivate ongoing developments. This trend won't just alter healthcare delivery; it may upend entire systems. What you read next might change how you see this forever. Prepare to have your preconceptions about telemedicine security blown away.
Telemedicine isn’t without obstacles. Speedy internet and device access remain issues for a large demographic, posing challenges for seamless adoption. Yet, the solution lies in ingenious tech solutions and a push toward universal access, a cause garnering global support. Even though the hardware hurdle remains, something remarkable is brewing under the surface.
A persistent challenge is the impersonal nature of digital consultations. Many fear losing the rapport traditionally built in-person. Yet, many specialists counter this with innovative engagement tactics, such as virtual care rooms designed to mimic face-to-face interactions. These surprising adaptations may be the key to reaching that familiarity gap.
Training and adaptability pose additional hurdles for both patients and healthcare professionals. Continuous education is vital to keeping up with evolving tools and methods, a task disproportionately affecting less tech-savvy individuals. But what’s most amazing is how communities are banding together to address these gaps with creative solutions.
The real twist is in the cultural shifts surrounding the practice. Traditional perceptions are evolving, pushing telemedicine toward the mainstream. Yet, the full impact of this growth is just beginning to unfold—what you’ll discover next will challenge the status quo of healthcare delivery as it stands today.
Economically, telemedicine holds both transformative potential and risk. While initial setup costs can be daunting, the long-term savings for healthcare systems are undeniable. Reform-driven experts are already mapping out potential budget reallocations that will change the face of funding strategies.

Moreover, telemedicine opens fertile ground for innovation and entrepreneurship. Startups are emerging, solving pressing healthcare needs with novel tech solutions. These ventures attract huge investments, indicating a growing faith in the telehealth market. But beyond the numbers lie untapped opportunities that might alter the competitive healthcare landscape dramatically.
Disparities in adoption rates represent a significant concern, posing questions about equitable access. Developing nations, in particular, face hurdles but find creative ways to leap ahead, turning potential roadblocks into unexpectedly positive scenarios. Watch how current technology paves new pathways for these global communities.
However, the ripple effects extend far beyond economics. As telehealth technologies become more ingrained in daily life, even non-healthcare sectors are noticing shifts. It’s these unnoticed changes that could serve as the seeds for the field’s most significant breakthroughs. What’s coming next will flip that switch in your perspective on telemedicine forever.
Through data analytics, telemedicine is advancing medical research flagrant with revelations. Massive datasets yield insights previously obscured by logistical challenges. With digital traces, patterns emerge that untangle long-standing medical mysteries. But the key breakthroughs are not solely from data; there’s a human element involved as well.

Digital consultations provide doctors with longitudinal data that’s visually intuitive. This in-depth view is pivotal in diagnosing complex conditions early, transforming patient treatment courses. Yet, few predict just how extensive the impact of this new wealth of data might extend. Is this the precursor to evolutionary shifts in medical practice?
Collaboration among specialists globally is now more feasible and beneficial. Professionals across various disciplines can now tackle complex cases together without geographical constraints. The synergy of these unions is leading to remarkable strides in solving health puzzles. The question that arises, though, is how regulatory technology will adapt to such evolving methodologies.
Real-world cases illustrate that this approach is more than theoretical. Successful outcomes are gaining higher recognition, but there’s room for even more hidden potential to surface. Discovering the next chapter in this journey could redefine our approach to healthcare universally.
Telemedicine has already begun altering existing regulatory frameworks. Policymakers worldwide are scrambling to keep pace with this rapid development. The legal landscape is adapting to complexities like cross-border consultations and online prescriptions, a process filled with hurdles and surprising discoveries.
One of the most intriguing prospects is the possibility of international telemedicine standards. These standards would harmonize practices across countries, allowing seamless professional activities and more fluid patient care. However, aligning these standards has proven to be more tangled than expected, raising intriguing debates about future collaborations.
Emerging technology also poses novel ethical dilemmas. Issues such as AI decision-making in clinical settings necessitate robust guidelines, reinforcing the need for proactive policymaking. But these ethical conundrums pose remarkable opportunities to redefine legal and moral standards in healthcare for future generations.
The race to innovate and regulate is a dynamic dance. With emerging insights, it’s clear that telemedicine’s potential knows no bounds. As the world adapts to these new paradigms, what’s around the corner in terms of policy evolution might just twist your mind into realizing that the very foundation of telemedicine is still under construction.
Telehealth fosters more than just access; it promotes health literacy. As patients take charge of their health data, the implication for empowered care is massive. The cultural shift toward e-health literacy is encouraging individuals to take proactive stances on personal wellbeing, a sea of change previously thought improbable.

The democratization of medical knowledge is eroding barriers, allowing previously underserved demographics a newfound power. The traditional doctor-patient hierarchy is undergoing a transformation, with shared decision-making becoming the new norm. Here’s the thought-provoking part: could this lead to patients becoming their own primary health advocates?
Moreover, tech learns from its users; telehealth platforms evolve through patient engagement. Feedback loops drive iterative improvements, making these tools better and more intuitive over time. This adaptation represents an unprecedented phenomenon where user experience significantly influences healthcare technology’s trajectory.
The shift's cultural impact extends beyond patients to professionals who embrace this new mode of practice. For skeptics, seeing the transformations in healthcare delivery first-hand can be mind-altering. In the coming paragraphs, what unfolds will show you a spectrum of possibilities you never envisioned at the start of this journey.
The clash and collaboration between traditional clinics and emerging telehealth platforms spark intriguing stories. These unexpected alliances have created synergies nobody anticipated, radically transforming how healthcare systems operate. At the onset, skepticism reigned, yet the results are undeniably advantageous.

Many argue that these partnerships offer the best of both worlds, providing flexibility while maintaining the accountability of brick-and-mortar institutions. It’s this collaborative potential that might pave pathways to new healthcare infrastructure. As you’ll see, real-world integration has surprising complexities.
Patients stand to gain significantly from these synergies. Yet, there’s a caveat: understanding each alliance’s scope remains crucial for maximizing the benefits while minimizing risk. Navigating these waters is a task of its own, ensuring partnerships remain productive without homogenizing experiences.
For those invested in telehealth’s future, examining these alliances is essential for understanding the full potential of modern medicine. As you continue exploring these chapters, what unravels is a world where the unknowns merge with the familiar in a dance of innovation and tradition. We’re peeling back one more layer to present you something even your doctor didn’t see coming.
While virtual consultations might be telemedicine’s face, the backend tech driving these interactions is evolving, making these services more effective than you might realize. Remote monitoring, AI-assisted diagnostics, and machine learning are redefining possibilities and outcomes.
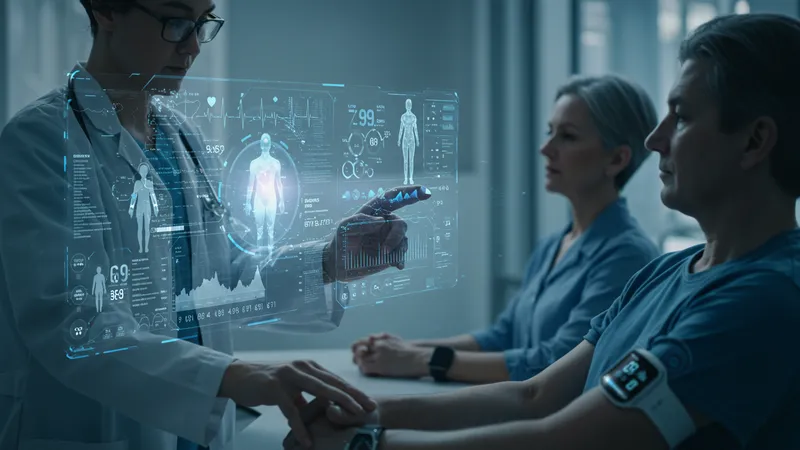
Huge strides are being made in integrating wearable tech with telehealth platforms. Devices tracking blood pressure, glucose levels, and heart rates send real-time data directly to physicians, augmenting chronic illness management. Yet, this is just scraping the surface of telecom-driven health data utilization.
Artificial intelligence is another game-changer, assisting in preventive care by predicting ailments before symptoms manifest. By leveraging big data, AI tailors individualized health advice, a process revolutionizing patient care but requiring meticulous checks for accuracy.
However, the best kept secret in telehealth might be digital therapeutics—apps and online programs representing a frontier of treatment options few understand yet. This potential paves new paths and questions about what we accept as conventional treatment modes. Can you imagine therapy without the therapy room? This is the new frontier.
Virtual clinics, once viewed skeptically, are gaining legitimacy as full-fledged medical entities. The infrastructure around these clinics is becoming sophisticated, with administrative supports closely mimicking those of physical offices, making these digital practices powerhouses of efficiency.
The virtual clinic model holds much promise for healthcare systems buckling under patient backlogs. These online spaces manage inflows intelligently, ensuring that patient care doesn’t compromise quality regardless of demand spikes. The scalability of virtual clinics is perhaps their most underestimated strength.
Interestingly, patient satisfaction rates soar in virtual setups due to improved access, continuous care, and swift professional communication. These positive outcomes challenge preconceived notions about virtual care’s efficacy compared to on-site consultations.
The question remains—how will physical clinics adapt to the escalating presence of their virtual counterparts? The answer may surprise you, forming a hybrid model that redefines not only how we receive care but also how we conceptualize what healthcare looks like in a digitized future.
Telemedicine’s reach spans demography and geography, appealing to diverse user groups from different walks of life. Older generations, initially apprehensive, now find value in improved access, prompting unique adoption trends among these historically tech-resistant groups.

Younger users, digital natives, are naturally drawn to the convenience offered by telehealth platforms, demanding seamless integration with tech-saturated lives. However, unearthing the hidden nuances of this demographic’s preferences provides further insights into evolving patient expectations.
This explosive growth is not limited to developed regions; developing nations are embracing telehealth with unexpected vigor. Innovations tailored to localized needs are catalyzing this growth, making telehealth a catalyst for change even in resource-limited settings.
For global adoption, scale remains vital. Still, skeptics question where balance lies between rapid growth and sustainable implementation. Unpacking these trends reveals solutions to challenges and opens doors to otherwise unconceivable possibilities for the future of medicine across the globe.
For practitioners, telemedicine offers both opportunities and challenges. Reduced overheads, flexible working conditions, and an expanded patient reach are among the triumphs often celebrated. Yet, the transition isn’t without its hurdles, requiring relentless adaptability.

Physicians grapple with technology fatigue as videoconferencing and data management become routine. Despite these strains, most agree that the pros outweigh the cons, a sentiment bolstered by rising job satisfaction reports.
Medics face another hurdle in sustaining clinical excellence. Ensuring high standards throughout online consultations can be a logistical test, pushing for innovative solutions and workarounds crucial to maintaining healthcare quality remotely.
What’s transparent, though, is the determination among healthcare professionals to harness telemedicine’s potential fully. Those succeeding in this domain are illuminated in roles adapting with unprecedented creativity. From their insights, the journey paves unforeseen options in traditional medical careers, reinvigorating the practice of modern healthcare.
For telehealth to sustain its growth, continuous medical education and training are pivotal. Virtual reality simulations, immersive tutorials, and AI-integrated learning modules offer promising solutions to keep healthcare professionals updated with lightning-fast advancements.

Institutions are adopting these innovations, recognizing the need for real-time, interactive learning. Yet, engagement levels among practitioners vary, sparking debates about best practices and effective learning paradigms in a digital teaching model.
The emphasis on telemedicine training extends beyond familiarity with tech platforms. Developing softer skills, like digital communication, is equally critical for maintaining patient rapport across virtual interfaces—a challenge some practitioners find surprisingly demanding.
Through constant training, professionals can uncover innovative opportunities hidden in the technological arsenal at their disposal. The rapid evolution of telemedicine necessitates this bullish approach to learning, implementing, and mastering. What remains a focus is protecting patients' interests while upholding the highest levels of care imaginable. And the tactics evolving next might just redefine this standard altogether.
As telemedicine rapidly expands, it presents novel ethical discussions surrounding equitable access and privacy concerns, redefining traditional ethics in delivering healthcare.
Practitioners face dilemmas of tech-induced choices for personal patient data, balancing ease of use with security safeguards. The struggle for ethical equilibrium hasn’t gone unnoticed.
Diverse cultural backgrounds shape varied perceptions, guiding discussions on delivering equitable, culturally sensitive online care, thus influencing service decisions at influential levels.
Thought leaders continue to delve into balancing convenience, accessibility, and privacy, formulating policies as pillars of digital ethics; their solutions may transform ethical healthcare standards moving forward.
Bringing resolution to these emerging challenges marks transformative cornerstones in telemedicine’s process, questioning frameworks yet refining protocols overall. The central query remains: how to cater ethically and comprehensively to tomorrow’s interconnected society powered by telemedicine?
The era of digital healthcare heralds unexpected yet thrilling innovations and breakthroughs that no one can ignore. From remote monitoring to AI-driven diagnostics and real-time data insights, telemedicine isn’t just about adapting—it’s about revolutionizing. And as this revolution gathers momentum, the seismic shift portends even more awe-inspiring transformations.
If the unexpected revelations and hidden potentials you’ve uncovered throughout this piece captivated you, don’t let the conversation end here. Share this article, bookmark your favorite sections, and take action because the future of healthcare is happening now and you’re a part of it. Stay informed and climate-ready for what promises to be the dawn of unprecedented digital health evolution.